One Man’s Story: ‘I took a mulligan on my vasectomy and got my third child.’

“I told my buddy, John, about my vasectomy reversal: ‘It was microsurgery. They wore high-powered microscope glasses.’ His smart-ass response: ‘Of course he did...for you!’ But John had no smart-ass response to offer once my third child—my post-vasectomy-reversal child—was born.” Tweet

Highlights
“I don’t care how many times you’ve tied a blood knot; vasectomy reversal doesn’t sound easy.”
“Reversals typically run $4,000 to $10,000, depending on the type of anesthesia you have. And it’s rarely covered by insurance.”
Dr. Larry Lipshultz: “Vas to vas, 95% [of reattachments] will have good semen quality.”
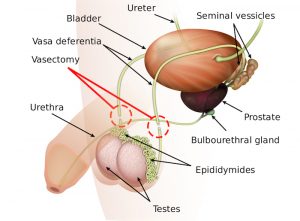
“...a vasectomy results in a backup of sperm that causes blockage on the side of the vas deferens attached to the epididymis...”
I told my buddy, John, about my vasectomy reversal: “It was microsurgery. The doctor wore these high-powered microscope glasses.”
“Of course, he did . . . for you!” He sniggered.
John, like many of my friends, needed an anatomy lesson. The vasa differentia: the two tubes that carry sperm from the epididymis to the ejaculatory duct are narrow—just about 4mm in diameter (thinner than a trout worm)—and surrounded by smooth muscle. Think of trying to tie together two ends of slippery fishing line attached to two egg sinkers.
Several factors can affect success rates: skill of the surgeon, type of surgery performed and number of years since the vasectomy.
“The monofilament surgical threads used to make a suture are basically a little thinner than a human hair,” says Larry Lipshultz, MD, world-renowned urologist and chief of the division of male-reproductive medicine and surgery at Baylor College of Medicine in Houston.
I don’t care how many times you’ve tied a blood knot, vasectomy reversal doesn’t sound easy.
“We do a two-layer procedure in that the vas is a very muscular tube with a small opening,” Dr. Lipshultz explained. “So, we first sew the opening together, and then we sew the outside together to make it watertight…takes about three hours. It enables us to offer fertility to a man who has previously elected to be sterilized.”
That was me.
I got my vasectomy a few months after the 9/11, terrorist attacks. My wife, Kathy, and I were still reeling from the horror that played out on our TV, and we decided we didn’t want to bring more children into such a dangerous world. Besides, we already had been blessed with two wonderful daughters. We were satisfied. And I rationalized it was my turn to take responsibility for birth control.
This surgery was different from my original snip-and-tuck—performed in a hospital—and a lot more expensive. Reversals typically run $4,000 to $10,000, depending on the type of anesthesia you have. And it’s rarely covered by insurance. Recovery, however, was similar to my vasectomy. I hung out on the couch, with a bag of frozen peas on my swollen scrotum, watching March Madness.
“Vas to vas, 95% [of reattachments] will have good semen quality,” Dr. Lipshultz said.
Several factors can affect success rates: skill of the surgeon, type of surgery performed and number of years since the vasectomy. Scar tissue may form and, with passage of time, can obstruct the opening. But Weill-Cornell University Medical Center’s Institute for Reproductive Medicine researchers in New York found that reversal success rates were still high—90% on average—up to 15 years after vasectomy, according to a study in The Journal of Urology.
“If a patient has a more complicated procedure and is concerned about failure, we can extract sperm at the time of reversal and bank it for them as kind of insurance,” Dr. Lipshultz added.
I had the standard vas repair, called a vasovasostomy. I choose to think my urologist was very skilled versus very lucky. He does just two reversals a year, he told me after the procedure.
I returned to the urologist’s office eight weeks later to provide a semen sample for analysis, which indicated success! My fish ladder had been fixed properly, and my swimmers were once again able to reach their spawning grounds.
Our family welcomed Sophia into the world about a year later, with immeasurable joy.
More From Larry I. Lipshultz, M.D.